Blood type

A blood type (also called a blood group) is a classification of blood based on the presence or absence of inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates, glycoproteins, or glycolipids, depending on the blood group system. Some of these antigens are also present on the surface of other types of cells of various tissues. Several of these red blood cell surface antigens that stem from one allele (or very closely linked genes), collectively form a blood group system.[1] Blood types are inherited and represent contributions from both parents. A total of 30 human blood group systems are now recognized by the International Society of Blood Transfusion (ISBT).[2]
Many pregnant women carry a fetus with a different blood type from their own, and the mother can form antibodies against fetal RBCs. Sometimes these maternal antibodies are IgG, a small immunoglobulin, which can cross the placenta and cause hemolysis of fetal RBCs, which in turn can lead to hemolytic disease of the newborn, an illness of low fetal blood counts that ranges from mild to severe.[3]
Contents |
Blood group systems
[2] A complete blood type would describe a full set of 30 substances on the surface of RBCs, and an individual's blood type is one of the many possible combinations of blood-group antigens. Across the 30 blood groups, over 600 different blood-group antigens have been found,[4] but many of these are very rare or are mainly found in certain ethnic groups.
Almost always, an individual has the same blood group for life, but very rarely an individual's blood type changes through addition or suppression of an antigen in infection, malignancy, or autoimmune disease.[5][6][7][8] An example of this rare phenomenon is the case of Demi-Lee Brennan, an Australian citizen, whose blood group changed after a liver transplant.[9][10] Another more common cause in blood-type change is a bone marrow transplant. Bone-marrow transplants are performed for many leukemias and lymphomas, among other diseases. If a person receives bone marrow from someone who is a different ABO type (e.g., a type A patient receives a type O bone marrow), the patient's blood type will eventually convert to the donor's type.
Some blood types are associated with inheritance of other diseases; for example, the Kell antigen is sometimes associated with McLeod syndrome.[11] Certain blood types may affect susceptibility to infections, an example being the resistance to specific malaria species seen in individuals lacking the Duffy antigen.[12] The Duffy antigen, presumably as a result of natural selection, is less common in ethnic groups from areas with a high incidence of malaria.[13]
ABO blood group system
The ABO system is the most important blood-group system in human-blood transfusion. The associated anti-A antibodies and anti-B antibodies are usually Immunoglobulin M, abbreviated IgM, antibodies. ABO IgM antibodies are produced in the first years of life by sensitization to environmental substances such as food, bacteria, and viruses. The O in ABO is often called 0 (zero, or null) in other languages.[14]
| Phenotype | Genotype |
|---|---|
| A | AA or AO |
| B | BB or BO |
| AB | AB |
| O | OO |
Rh blood group system
The Rh system is the second most significant blood-group system in human-blood transfusion with currently 50 antigens. The most significant Rh antigen is the D antigen because it is the most likely to provoke an immune system response of the five main Rh antigens. It is common for D-negative individuals not to have any anti-D IgG or IgM antibodies, because anti-D antibodies are not usually produced by sensitization against environmental substances. However, D-negative individuals can produce IgG anti-D antibodies following a sensitizing event: possibly a fetomaternal transfusion of blood from a fetus in pregnancy or occasionally a blood transfusion with D positive RBCs.[15] Rh disease can develop in these cases.[16] Rh negative blood types are much less in proportion of Asian populations (0.3%) than they are in White (15%).[17] In the table below, the presence or absence of the Rh antigens is signified by the + or - sign, so that for example A- group does not have any of the Rh antigens.
ABO and Rh distribution by country
| Country | Population[18] | O+ | A+ | B+ | AB+ | O- | A- | B- | AB- |
|---|---|---|---|---|---|---|---|---|---|
| Australia[19] | 21,262,641 | 40% | 31% | 8% | 2% | 9% | 7% | 2% | 1% |
| Austria[20] | 8,210,281 | 30% | 33% | 12% | 6% | 7% | 8% | 3% | 1% |
| Belgium[21] | 10,414,336 | 38% | 34% | 8.5% | 4.1% | 7% | 6% | 1.5% | 0.8% |
| Brazil[22] | 198,739,269 | 36% | 34% | 8% | 2.5% | 9% | 8% | 2% | 0.5% |
| Canada[23] | 33,487,208 | 39% | 36% | 7.6% | 2.5% | 7% | 6% | 1.4% | 0.5% |
| Denmark[24] | 5,500,510 | 35% | 37% | 8% | 4% | 6% | 7% | 2% | 1% |
| Estonia[25] | 1,299,371 | 30% | 31% | 20% | 6% | 4.5% | 4.5% | 3% | 1% |
| Finland[26] | 5,250,275 | 27% | 38% | 15% | 7% | 4% | 6% | 2% | 1% |
| France[27] | 62,150,775 | 36% | 37% | 9% | 3% | 6% | 7% | 1% | 1% |
| Germany[28] | 82,329,758 | 35% | 37% | 9% | 4% | 6% | 6% | 2% | 1% |
| Hong Kong SAR[29] | 7,055,071 | 10% | 26% | 27% | 7% | 0.31% | 0.19% | 0.14% | 0.05% |
| Iceland[30] | 306,694 | 47.6% | 26.4% | 9.3% | 1.6% | 8.4% | 4.6% | 1.7% | 0.4% |
| India[31] | 1,166,079,217 | 36.5% | 22.1% | 30.9% | 6.4% | 2.0% | 0.8% | 1.1% | 0.2% |
| Iran[32] | 75,222,200 | 55% | 6% | 9% | 1% | 5% | 5% | 2% | 1% |
| Ireland[33] | 4,203,200 | 47% | 26% | 9% | 2% | 8% | 5% | 2% | 1% |
| Israel[34] | 7,233,701 | 32% | 34% | 17% | 7% | 3% | 4% | 2% | 1% |
| Netherlands[35] | 16,715,999 | 39.5% | 35% | 6.7% | 2.5% | 7.5% | 7% | 1.3% | 0.5% |
| New Zealand[36] | 4,213,418 | 38% | 32% | 9% | 3% | 9% | 6% | 2% | 1% |
| Norway[37] | 4,660,539 | 34% | 42.5% | 6.8% | 3.4% | 6% | 7.5% | 1.2% | 0.6% |
| Poland[38] | 38,482,919 | 31% | 32% | 15% | 7% | 6% | 6% | 2% | 1% |
| Portugal[39] | 10,707,924 | 36.2% | 39.8% | 6.6% | 2.9% | 6.0% | 6.6% | 1.1% | 0.5% |
| Saudi Arabia[40] | 28,686,633 | 48% | 24% | 17% | 4% | 4% | 2% | 1% | 0.23% |
| South Africa[41] | 49,320,000 | 39% | 32% | 12% | 3% | 7% | 5% | 2% | 1% |
| Spain[42] | 40,525,002 | 36% | 34% | 8% | 2.5% | 9% | 8% | 2% | 0.5% |
| Sweden[43] | 9,059,651 | 32% | 37% | 10% | 5% | 6% | 7% | 2% | 1% |
| Taiwan[44] | 24,000,000 | 43.9% | 25.9% | 23.9% | 6.0% | 0.1% | 0.1% | 0.01% | 0.02% |
| Turkey[45] | 76,805,524 | 29.8% | 37.8% | 14.2% | 7.2% | 3.9% | 4.7% | 1.6% | 0.8% |
| United Kingdom[46] | 61,113,205 | 37% | 35% | 8% | 3% | 7% | 7% | 2% | 1% |
| United States[47] | 307,212,123 | 37.4% | 35.7% | 8.5% | 3.4% | 6.6% | 6.3% | 1.5% | 0.6% |
| Population-weighted mean | (total population = 2,261,025,244) | 36.44% | 28.27% | 20.59% | 5.06% | 4.33% | 3.52% | 1.39% | 0.45% |
| Racial and ethnic distribution of ABO (without Rh) blood types[48] (This table has more entries than the table above but does not distinguish between Rh types.) |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Blood group B has its highest frequency in Northern India and neighboring Central Asia, and its incidence diminishes both towards the west and the east, falling to single digit percentages in Spain.[49][50] It is believed to have been entirely absent from Native American and Australian Aboriginal populations prior to the arrival of Europeans in those areas.[50][51]
Blood group A is associated with high frequencies in Europe, especially in Scandinavia and Central Europe, although its highest frequencies occur in some Australian Aborigine populations and the Blackfoot Indians of Montana.[52][53]
Other blood group systems
The International Society of Blood Transfusion currently recognizes 30 blood-group systems (including the ABO and Rh systems).[2] Thus, in addition to the ABO antigens and Rh antigens, many other antigens are expressed on the RBC surface membrane. For example, an individual can be AB, D positive, and at the same time M and N positive (MNS system), K positive (Kell system), Lea or Leb negative (Lewis system), and so on, being positive or negative for each blood group system antigen. Many of the blood group systems were named after the patients in whom the corresponding antibodies were initially encountered.
Clinical significance
Blood transfusion
Transfusion medicine is a specialized branch of hematology that is concerned with the study of blood groups, along with the work of a blood bank to provide a transfusion service for blood and other blood products. Across the world, blood products must be prescribed by a medical doctor (licensed physician or surgeon) in a similar way as medicines.
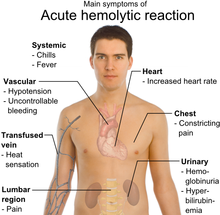
Much of the routine work of a blood bank involves testing blood from both donors and recipients to ensure that every individual recipient is given blood that is compatible and is as safe as possible. If a unit of incompatible blood is transfused between a donor and recipient, a severe acute hemolytic reaction with hemolysis (RBC destruction), renal failure and shock is likely to occur, and death is a possibility. Antibodies can be highly active and can attack RBCs and bind components of the complement system to cause massive hemolysis of the transfused blood.
Patients should ideally receive their own blood or type-specific blood products to minimize the chance of a transfusion reaction. Risks can be further reduced by cross-matching blood, but this may be skipped when blood is required for an emergency. Cross-matching involves mixing a sample of the recipient's serum with a sample of the donor's red blood cells and checking if the mixture agglutinates, or forms clumps. If agglutination is not obvious by direct vision, blood bank technicians usually check for agglutination with a microscope. If agglutination occurs, that particular donor's blood cannot be transfused to that particular recipient. In a blood bank it is vital that all blood specimens are correctly identified, so labeling has been standardized using a barcode system known as ISBT 128.
The blood group may be included on identification tags or on tattoos worn by military personnel, in case they should need an emergency blood transfusion. Frontline German Waffen-SS had blood group tattoos during World War II.
Rare blood types can cause supply problems for blood banks and hospitals. For example Duffy-negative blood occurs much more frequently in people of African origin,[56] and the rarity of this blood type in the rest of the population can result in a shortage of Duffy-negative blood for patients of African ethnicity. Similarly for RhD negative people, there is a risk associated with travelling to parts of the world where supplies of RhD negative blood are rare, particularly East Asia, where blood services may endeavor to encourage Westerners to donate blood.[57]
Hemolytic disease of the newborn (HDN)
A pregnant woman can make IgG blood group antibodies if her fetus has a blood group antigen that she does not have. This can happen if some of the fetus' blood cells pass into the mother's blood circulation (e.g. a small fetomaternal hemorrhage at the time of childbirth or obstetric intervention), or sometimes after a therapeutic blood transfusion. This can cause Rh disease or other forms of hemolytic disease of the newborn (HDN) in the current pregnancy and/or subsequent pregnancies. If a pregnant woman is known to have anti-D antibodies, the Rh blood type of a fetus can be tested by analysis of fetal DNA in maternal plasma to assess the risk to the fetus of Rh disease.[58] One of the major advances of twentieth century medicine was to prevent this disease by stopping the formation of Anti-D antibodies by D negative mothers with an injectable medication called Rho(D) immune globulin.[59][60] Antibodies associated with some blood groups can cause severe HDN, others can only cause mild HDN and others are not known to cause HDN.[3]
Blood products
To provide maximum benefit from each blood donation and to extend shelf-life, blood banks fractionate some whole blood into several products. The most common of these products are packed RBCs, plasma, platelets, cryoprecipitate, and fresh frozen plasma (FFP). FFP is quick-frozen to retain the labile clotting factors V and VIII, which are usually administered to patients who have a potentially fatal clotting problem caused by a condition such as advanced liver disease, overdose of anticoagulant, or disseminated intravascular coagulation (DIC)
Units of packed red cells are made by removing as much of the plasma as possible from whole blood units.
Clotting factors synthesized by modern recombinant methods are now in routine clinical use for hemophilia, as the risks of infection transmission that occur with pooled blood products are avoided.
Red blood cell compatibility
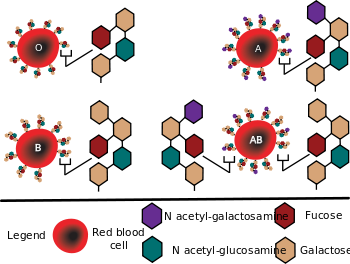
- Blood group AB individuals have both A and B antigens on the surface of their RBCs, and their blood serum does not contain any antibodies against either A or B antigen. Therefore, an individual with type AB blood can receive blood from any group (with AB being preferable), but can donate blood only to another type AB individual.
- Blood group A individuals have the A antigen on the surface of their RBCs, and blood serum containing IgM antibodies against the B antigen. Therefore, a group A individual can receive blood only from individuals of groups A or O (with A being preferable), and can donate blood to individuals with type A or AB.
- Blood group B individuals have the B antigen on the surface of their RBCs, and blood serum containing IgM antibodies against the A antigen. Therefore, a group B individual can receive blood only from individuals of groups B or O (with B being preferable), and can donate blood to individuals with type B or AB.
- Blood group O (or blood group zero in some countries) individuals do not have either A or B antigens on the surface of their RBCs, but their blood serum contains IgM anti-A antibodies and anti-B antibodies against the A and B blood group antigens. Therefore, a group O individual can receive blood only from a group O individual, but can donate blood to individuals of any ABO blood group (i.e. A, B, O or AB). If anyone needs a blood transfusion in an extremely dire emergency, and if the time taken to process the recipient's blood would cause a detrimental delay, O Negative blood can be issued.

In addition to donating to the same blood group; type O blood donors can give to A, B and AB; blood donors of types A and B can give to AB.
| Recipient[1] | Donor[1] | |||||||
|---|---|---|---|---|---|---|---|---|
| O− | O+ | A− | A+ | B− | B+ | AB− | AB+ | |
| O− | ||||||||
| O+ | ||||||||
| A− | ||||||||
| A+ | ||||||||
| B− | ||||||||
| B+ | ||||||||
| AB− | ||||||||
| AB+ | ||||||||
Table note
1. Assumes absence of atypical antibodies that would cause an incompatibility between donor and recipient blood, as is usual for blood selected by cross matching.
An Rh D-negative patient who does not have any anti-D antibodies (never being previously sensitized to D-positive RBCs) can receive a transfusion of D-positive blood once, but this would cause sensitization to the D antigen, and a female patient would become at risk for hemolytic disease of the newborn. If a D-negative patient has developed anti-D antibodies, a subsequent exposure to D-positive blood would lead to a potentially dangerous transfusion reaction. Rh D-positive blood should never be given to D-negative women of child bearing age or to patients with D antibodies, so blood banks must conserve Rh-negative blood for these patients. In extreme circumstances, such as for a major bleed when stocks of D-negative blood units are very low at the blood bank, D-positive blood might be given to D-negative females above child-bearing age or to Rh-negative males, providing that they did not have anti-D antibodies, to conserve D-negative blood stock in the blood bank. The converse is not true; Rh D-positive patients do not react to D negative blood. This same matching is done for other antigens of the Rh system as C, c, E and e and for other blood group systems with a known risk for immunization such as the Kell system in particular for females of child-bearing age or patients with known need for many transfusions.
Plasma compatibility

In addition to donating to the same blood group; plasma from type AB can be given to A, B and O; plasma from types A and B can be given to O.
Recipients can receive plasma of the same blood group, but otherwise the donor-recipient compatibility for blood plasma is the converse of that of RBCs: plasma extracted from type AB blood can be transfused to individuals of any blood group; individuals of blood group O can receive plasma from any blood group; and type O plasma can be used only by type O recipients.
| Recipient | Donor[1] | |||
|---|---|---|---|---|
| O | A | B | AB | |
| O | ||||
| A | ||||
| B | ||||
| AB | ||||
Table note
1. Assumes absence of strong atypical antibodies in donor plasma
Rh D antibodies are uncommon, so generally neither D negative nor D positive blood contain anti-D antibodies. If a potential donor is found to have anti-D antibodies or any strong atypical blood group antibody by antibody screening in the blood bank, they would not be accepted as a donor (or in some blood banks the blood would be drawn but the product would need to be appropriately labeled); therefore, donor blood plasma issued by a blood bank can be selected to be free of D antibodies and free of other atypical antibodies, and such donor plasma issued from a blood bank would be suitable for a recipient who may be D positive or D negative, as long as blood plasma and the recipient are ABO compatible.
Universal donors and universal recipients

With regard to transfusions of whole blood or packed red blood cells, individuals with type O Rh D negative blood are often called universal donors, and those with type AB Rh D positive blood are called universal recipients; however, these terms are only generally true with respect to possible reactions of the recipient's anti-A and anti-B antibodies to transfused red blood cells, and also possible sensitization to Rh D antigens. One exception is individuals with hh antigen system (also known as the Bombay blood group) who can only receive blood safely from other hh donors, because they form antibodies against the H substance.[63][64]
Blood donors with particularly strong anti-A, anti-B or any atypical blood group antibody are excluded from blood donation. The possible reactions of anti-A and anti-B antibodies present in the transfused blood to the recipients RBCs need not be considered, because a relatively small volume of plasma containing antibodies is transfused.
By way of example: considering the transfusion of O Rh D negative blood (universal donor blood) into a recipient of blood group A Rh D positive, an immune reaction between the recipient's anti-B antibodies and the transfused RBCs is not anticipated. However, the relatively small amount of plasma in the transfused blood contains anti-A antibodies, which could react with the A antigens on the surface of the recipients RBCs, but a significant reaction is unlikely because of the dilution factors. Rh D sensitization is not anticipated.
Additionally, red blood cell surface antigens other than A, B and Rh D, might cause adverse reactions and sensitization, if they can bind to the corresponding antibodies to generate an immune response. Transfusions are further complicated because platelets and white blood cells (WBCs) have their own systems of surface antigens, and sensitization to platelet or WBC antigens can occur as a result of transfusion.
With regard to transfusions of plasma, this situation is reversed. Type O plasma, containing both anti-A and anti-B antibodies, can only be given to O recipients. The antibodies will attack the antigens on any other blood type. Conversely, AB plasma can be given to patients of any ABO blood group due to not containing any anti-A or anti-B antibodies.
Blood group genotyping
In addition to the current practice of serologic testing of blood types, the progress in molecular diagnostics allows the increasing use of blood group genotyping. In contrast to serologic tests reporting a direct blood type phenotype, genotyping allows the prediction of a phenotype based on the knowledge of the molecular basis of the currently known antigens. This allows a more detailed determination of the blood type and therefore a better match for transfusion, which can be crucial in particular for patients with needs for many transfusions to prevent allo-immunization.[65][66]
Conversion
In April 2007, a method was discovered to convert blood types A, B, and AB to O, using enzymes. This method is still experimental and the resulting blood has yet to undergo human trials.[67][68] The method specifically removes or converts antigens on the red blood cells, so other antigens and antibodies would remain. This does not help plasma compatibility, but that is a lesser concern since plasma has much more limited clinical utility in transfusion and is much easier to preserve.
History
The two most significant blood group systems were discovered by Karl Landsteiner during early experiments with blood transfusion: the ABO group in 1901[69] and in co-operation with Alexander S. Wiener the Rhesus group in 1937.[70] Development of the Coombs test in 1945,[71] the advent of transfusion medicine, and the understanding of hemolytic disease of the newborn led to discovery of more blood groups, and now 30 human blood group systems are recognized by the International Society of Blood Transfusion (ISBT),[2] and across the 30 blood groups, over 600 different blood group antigens have been found,[4] many of these are very rare or are mainly found in certain ethnic groups. Blood types have been used in forensic science and in paternity testing, but both of these uses are being replaced by genetic fingerprinting, which provides greater certainty.[72]
Cultural beliefs and other claims
A popular belief in Japan is that a person's ABO blood type is predictive of their personality, character, and compatibility with others. This belief is also widespread in South Korea.[73] Deriving from ideas of historical scientific racism, the theory reached Japan in a 1927 psychologist's report, and the militarist government of the time commissioned a study aimed at breeding better soldiers.[73] The fad faded in the 1930s due to its unscientific basis. The theory has long since been rejected by the scientists, but it was revived in the 1970s by Masahiko Nomi, a broadcaster who had no medical background.[73]
References
- ↑ Maton, Anthea; Jean Hopkins, Charles William McLaughlin, Susan Johnson, Maryanna Quon Warner, David LaHart, Jill D. Wright (1993). Human Biology and Health. Englewood Cliffs, New Jersey, USA: Prentice Hall. ISBN 0-13-981176-1.
- ↑ 2.0 2.1 2.2 2.3 "Table of blood group systems". International Society of Blood Transfusion. October 2008. http://ibgrl.blood.co.uk/isbt%20pages/isbt%20terminology%20pages/table%20of%20blood%20group%20systems.htm. Retrieved 2008-09-12.
- ↑ 3.0 3.1 E.A. Letsky; I. Leck, J.M. Bowman (2000). "Chapter 12: Rhesus and other haemolytic diseases". Antenatal & neonatal screening (Second ed.). Oxford University Press. ISBN 0-19-262827-7.
- ↑ 4.0 4.1 "American Red Cross Blood Services, New England Region, Maine, Massachusetts, New Hampshire, Vermont". American Red Cross Blood Services - New England Region. 2001. http://www.newenglandblood.org/medical/rare.htm. Retrieved 2008-07-15. "there are more than 600 known antigens besides A and B that characterize the proteins found on a person's red cells"
- ↑ Dean, Laura. "The ABO blood group". Blood Groups and Red Cell Antigens. online: NCBI. http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=rbcantigen&part=ch05ABO. "A number of illnesses may alter a person's ABO phenotype"
- ↑ Stayboldt C, Rearden A, Lane TA (1987). "B antigen acquired by normal A1 red cells exposed to a patient's serum". Transfusion 27 (1): 41–4. doi:10.1046/j.1537-2995.1987.27187121471.x. PMID 3810822.
- ↑ Matsushita S, Imamura T, Mizuta T, Hanada M (November 1983). "Acquired B antigen and polyagglutination in a patient with gastric cancer". The Japanese Journal of Surgery 13 (6): 540–2. doi:10.1007/BF02469500. PMID 6672386.
- ↑ Kremer Hovinga I, Koopmans M, de Heer E, Bruijn J, Bajema I (2007). "Change in blood group in systemic lupus erythematosus". Lancet 369 (9557): 186–7; author reply 187. doi:10.1016/S0140-6736(07)60099-3. PMID 17240276.
- ↑ Demi-Lee Brennan has changed blood types and immune system Kate Sikora, The Daily Telegraph, January 25, 2008
- ↑ Aust doctors hail teen's transplant 'miracle' Sean Rubinsztein-Dunlop, ABC News (Australia), January 24, 2008
- ↑ Chown B., Lewis M., Kaita K. (October 1957). "A new Kell blood-group phenotype". Nature 180 (4588): 711. doi:10.1038/180711a0. PMID 13477267.
- ↑ Miller LH, Mason SJ, Clyde DF, McGinniss MH (August 1976). "The resistance factor to Plasmodium vivax in blacks. The Duffy-blood-group genotype, FyFy". The New England Journal of Medicine 295 (6): 302–4. PMID 778616.
- ↑ Kwiatkowski DP (August 2005). "How malaria has affected the human genome and what human genetics can teach us about malaria". American Journal of Human Genetics 77 (2): 171–92. doi:10.1086/432519. PMID 16001361. "The different geographic distributions of α thalassemia, G6PD deficiency, ovalocytosis, and the Duffy-negative blood group are further examples of the general principle that different populations have evolved different genetic variants to protect against malaria".
- ↑ "Your blood – a textbook about blood and blood donation" (PDF). p. 63. http://www.bloddonor.dk/fileadmin/Fil_Arkiv/PDF_filer/Andre/Your_Blood__June_2006.pdf. Retrieved 2008-07-15.
- ↑ Talaro, Kathleen P. (2005). Foundations in microbiology (5th ed.). New York: McGraw-Hill. pp. 510–1. ISBN 0-07-111203-0.
- ↑ Moise KJ (July 2008). "Management of rhesus alloimmunization in pregnancy". Obstetrics and Gynecology 112 (1): 164–76. doi:10.1097/AOG.0b013e31817d453c. PMID 18591322.
- ↑ "Rh血型的由來". Hospital.kingnet.com.tw. http://hospital.kingnet.com.tw/activity/blood/html/a.html. Retrieved 2010-08-01.
- ↑ CIA World Factbook
- ↑ "Blood Types - What Are They?, Australian Red Cross". Giveblood.redcross.org.au. http://www.giveblood.redcross.org.au/page.aspx?IDDataTreeMenu=42&parent=30. Retrieved 2010-08-01.
- ↑ "Austrian Red Cross - Blood Donor Information". Old.roteskreuz.at. 2006-03-21. http://old.roteskreuz.at/47_body.html#blutgruppen. Retrieved 2010-08-01.
- ↑ "Rode Kruis Wielsbeke - Blood Donor information material". Rodekruiswielsbeke.be. http://www.rodekruiswielsbeke.be/infobloed.html. Retrieved 2010-08-01.
- ↑ Tipos Sanguíneos
- ↑ Canadian Blood Services - Société canadienne du sang. "Types & Rh System, Canadian Blood Services". Bloodservices.ca. http://www.bloodservices.ca/CentreApps/Internet/UW_V502_MainEngine.nsf/page/Blood%20Types%20and%20Rh%20System?OpenDocument. Retrieved 2010-08-01.
- ↑ Frequency of major blood groups in the Danish population.
- ↑ "Veregruppide esinemissagedus Eestis". Kliinikum.ee. http://www.kliinikum.ee/verekeskus/index.php?menu=9&mod=page&id=5. Retrieved 2010-08-01.
- ↑ "Suomalaisten veriryhmäjakauma". Veripalvelu.fi. 2009-08-21. http://www.veripalvelu.fi/asp/system/empty.asp?P=1275&VID=default&SID=908029945449597&S=1&C=24395. Retrieved 2010-08-01.
- ↑ "Les groupes sanguins (système ABO)" (in French). Centre Hospitalier Princesse Grace - Monaco. C.H.P.G. MONACO. 2005. http://www.chpg.mc/go/article.php3?id_article=111. Retrieved 2008-07-15.
- ↑ Häufigkeit der Blutgruppen
- This article incorporates information from the German Wikipedia.
- ↑ Blood Donation, Hong Kong Red Cross
- ↑ "Blóðflokkar". Landspitali.is. http://www4.landspitali.is/lsh_ytri.nsf/pages/bb_blodflokkarnir. Retrieved 2010-08-01.
- ↑ "Indian Journal for the Practising Doctor". Indmedica.com. http://www.indmedica.com/journals.php?journalid=3&issueid=75&articleid=965&action=article. Retrieved 2010-08-01.
- ↑ "Irish Blood Transfusion Service - Irish Blood Group Type Frequency Distribution". Irish Blood Transfusion Service. http://www.ibts.ie/All_About_Blood/Blood_Group_Basics/. Retrieved 2009-11-07.
- ↑ "Irish Blood Transfusion Service - Irish Blood Group Type Frequency Distribution". Irish Blood Transfusion Service. http://www.ibts.ie/All_About_Blood/Blood_Group_Basics/. Retrieved 2009-11-07.
- ↑ "The national rescue service in Israel". Mdais.org. http://www.mdais.org/362/. Retrieved 2010-08-01.
- ↑ "Voorraad Erytrocytenconcentraten Bij Sanquin" (in Dutch). http://www.sanquin.nl/Sanquin-nl/erygrafiek.nsf/All/Voorraad-Erytrocytenconcentraten-Bij-Sanquin.html. Retrieved 2009-03-27.
- ↑ "What are Blood Groups?". NZ Blood. http://www.nzblood.co.nz/?t=31. Retrieved 2010-08-01.
- ↑ Norwegian Blood Donor Organization
- ↑ "Regionalne Centrum Krwiodawstwa i Krwiolecznictwa we Wroclawiu". Rckik.wroclaw.pl. 2010-07-20. http://rckik.wroclaw.pl/?id=5&go=0. Retrieved 2010-08-01.
- ↑ Portuguese Blood Institute (assuming Rh and AB antigens are independent)
- ↑ "Fequency of ABO blood groups in the eastern region of Saudi Arabia". Cat.inist.fr. http://cat.inist.fr/?aModele=afficheN&cpsidt=14126617. Retrieved 2010-08-01.
- ↑ "South African National Blood Service - What's Your Type?". Sanbs.org.za. http://www.sanbs.org.za/donors_whattype.htm. Retrieved 2010-08-01.
- ↑ "Federación Nacional de Donantes de Sangre/La sangre/Grupos". Donantesdesangre.net. http://www.donantesdesangre.net/menu.htm. Retrieved 2010-08-01.
- ↑ "Frequency of major blood groups in the Swedish population". Geblod.nu. 2007-10-02. http://www.geblod.nu/general.aspx?PageId=10. Retrieved 2010-08-01.
- ↑ "Rh血型的由來". Hospital.kingnet.com.tw. http://hospital.kingnet.com.tw/activity/blood/html/a.html. Retrieved 2010-08-01.
- ↑ "Turkey Blood Group Site". Kangrubu.com. http://www.kangrubu.com/default.asp?sayfa=kan_gruplari. Retrieved 2010-08-01.
- ↑ "Frequency of major blood groups in the UK". Blood.co.uk. http://www.blood.co.uk/pages/all_about.html. Retrieved 2010-08-01.
- ↑ "Blood Types in the U.S". Bloodcenter.stanford.edu. 2008-06-20. http://bloodcenter.stanford.edu/about_blood/blood_types.html. Retrieved 2010-08-01.
- ↑ "Racial and ethnic distribution of ABO blood types". Bloodbook.com. http://www.bloodbook.com/world-abo.html. Retrieved 2010-08-01.
- ↑ Blood Transfusion Division, United States Army Medical Research Laboratory (1971). Selected contributions to the literature of blood groups and immunology. 1971 v. 4. United States Army Medical Research Laboratory, Fort Knox, Kentucky. http://books.google.com/?id=ALilcA7Acd0C. "... In northern India, in Southern and Central China and in the neighboring Central Asiatic areas, we find the highest known frequencies of B. If we leave this center, the frequency of the B gene decreases almost everywhere ..."
- ↑ 50.0 50.1 Encyclopaedia Britannica (2002). The New Encyclopaedia Britannica. Encyclopaedia Britannica, Inc.. ISBN 0852297874. http://books.google.com/?id=fpdUAAAAMAAJ. "... The maximum frequency of the B gene occurs in Central Asia and northern India. The B gene was probably absent from American Indians and Australian Aborigines before racial admixture occurred with the coming of the white man ..."
- ↑ Carol R. Ember, Melvin Ember (1973). Anthropology. Appleton-Century-Crofts. http://books.google.com/?id=fvpFAAAAMAAJ. "... Blood type B is completely absent in most North and South American Indians ..."
- ↑ Laura Dean, MD (2005). Blood Groups an Red Cell Antigens. National Center for Biotechnology Information, United States Government. ISBN 1932811052. http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=rbcantigen. "... Type A is common in Central and Eastern Europe. In countries such as Austria, Denmark, Norway, and Switzerland, about 45-50% of the population have this blood type, whereas about 40% of Poles and Ukrainians do so. The highest frequencies are found in small, unrelated populations. For example, about 80% of the Blackfoot Indians of Montana have blood type A ..."
- ↑ (PDF) Technical Monograph No. 2: The ABO Blood Group System and ABO Subgroups. Biotec. March 2005. http://www.biotec.com/pdf/Technical%20Monograph%20No.%202%20-%20ABO%20system%20and%20subgroups.pdf. "... The frequency of blood group A is quite high (25-55%) in Europe, especially in Scandinavia and parts of central Europe. High group A frequency is also found in the Aborigines of South Australia (up to 45%) and in certain American Indian tribes where the frequency reaches 35% ..."
- ↑ Possible Risks of Blood Product Transfusions from American Cancer Society. Last Medical Review: 03/08/2008. Last Revised: 01/13/2009
- ↑ 7 adverse reactions to transfusion Pathology Department at University of Michigan. Version July 2004, Revised 11/5/08
- ↑ Nickel RG, Willadsen SA, Freidhoff LR, et al. (August 1999). "Determination of Duffy genotypes in three populations of African descent using PCR and sequence-specific oligonucleotides". Human Immunology 60 (8): 738–42. doi:10.1016/S0198-8859(99)00039-7. PMID 10439320.
- ↑ Bruce, MG (May 2002). "BCF - Members - Chairman's Annual Report". The Blood Care Foundation. http://www.bloodcare.org.uk/html/resources_chairman_2001.htm. Retrieved 2008-07-15. "As Rhesus Negative blood is rare amongst local nationals, this Agreement will be of particular value to Rhesus Negative expatriates and travellers"
- ↑ Daniels G, Finning K, Martin P, Summers J (September 2006). "Fetal blood group genotyping: present and future". Annals of the New York Academy of Sciences 1075: 88–95. doi:10.1196/annals.1368.011. PMID 17108196.
- ↑ "Use of Anti-D Immunoglobulin for Rh Prophylaxis". Royal College of Obstetricians and Gynaecologists. May 2002. http://www.rcog.org.uk/index.asp?PageID=1972.
- ↑ "Pregnancy - routine anti-D prophylaxis for D-negative women". NICE. May 2002. http://www.nice.org.uk/guidance/TA41/?c=91520.
- ↑ "RBC compatibility table". American National Red Cross. December 2006. http://chapters.redcross.org/br/northernohio/INFO/bloodtype.html. Retrieved 2008-07-15.
- ↑ 62.0 62.1 Blood types and compatibility bloodbook.com
- ↑ Fauci, Anthony S.; Eugene Braunwald, Kurt J. Isselbacher, Jean D. Wilson, Joseph B. Martin, Dennis L. Kasper, Stephen L. Hauser, Dan L. Longo (1998). Harrison's Principals of Internal Medicine. New York: McGraw-Hill. pp. 719.. ISBN 0-07-020291-5.)
- ↑ "Universal acceptor and donor groups". Webmd.com. 2008-06-12. http://www.webmd.com/a-to-z-guides/blood-type-test. Retrieved 2010-08-01.
- ↑ Anstee DJ (2009). "Red cell genotyping and the future of pretransfusion testing". Blood 114 (2): 248–56. doi:10.1182/blood-2008-11-146860. PMID 19411635.
- ↑ Avent ND (2009). "Large-scale blood group genotyping: clinical implications". Br J Haematol 144 (1): 3–13. doi:10.1111/j.1365-2141.2008.07285.x. PMID 19016734.
- ↑ "Blood groups 'can be converted'". BBC News. 2007-04-02. http://news.bbc.co.uk/1/hi/health/6517137.stm. Retrieved 2008-07-15.
- ↑ Liu Q, Sulzenbacher G, Yuan H, Bennett E, Pietz G, Saunders K, Spence J, Nudelman E, Levery S, White T, Neveu J, Lane W, Bourne Y, Olsson M, Henrissat B, Clausen H (2007). "Bacterial glycosidases for the production of universal red blood cells". Nat Biotechnol 25 (4): 454. doi:10.1038/nbt1298. PMID 17401360.
- ↑ Landsteiner K. Zur Kenntnis der antifermentativen, lytischen und agglutinierenden Wirkungen des Blutserums und der Lymphe. Zentralblatt Bakteriologie 1900;27:357-62.
- ↑ Landsteiner K, Wiener AS. An agglutinable factor in human blood recognized by immune sera for rhesus blood. Proc Soc Exp Biol Med 1940;43:223-224.
- ↑ Coombs RRA, Mourant AE, Race RR. A new test for the detection of weak and "incomplete" Rh agglutinins. Brit J Exp Path 1945;26:255-66.
- ↑ Johnson P, Williams R, Martin P (2003). "Genetics and Forensics: Making the National DNA Database". Science Studies 16 (2): 22–37. PMID 16467921.
- ↑ 73.0 73.1 73.2 "Myth about Japan blood types under attack". Associated Press. AOL Health. 2005-05-06. http://aol.mediresource.com/channel_health_news_details.asp?news_id=6661&news_channel_id=11&channel_id=11. Retrieved 2007-12-29.
Further reading
- Dean, Laura. "Blood Groups and Red Cell Antigens, a guide to the differences in our blood types that complicate blood transfusions and pregnancy." (HTML, also PDF, Flash and PRC versions). National Center for Biotechnology Information. http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=rbcantigen. Retrieved September 15, 2006.
- Mollison PL, Engelfriet CP and Contreras M. Blood Transfusion in Clinical Medicine. 1997. 10th edition. Blackwell Science, Oxford, UK. ISBN 0-86542-881-6.
External links
- BGMUT Blood Group Antigen Gene Mutation Database at NCBI, NIH has details of genes and proteins, and variations thereof, that are responsible for blood types
- Online 'Mendelian Inheritance in Man' (OMIM) 110300 (ABO)
- Online 'Mendelian Inheritance in Man' (OMIM) 111680 (Rhesus D)
- Farr AD (April 1979). "Blood group serology--the first four decades (1900--1939)". Medical History 23 (2): 215–26. PMID 381816.
- "Blood group test, Gentest.ch" (HTML, JavaScript). Gentest.ch GmbH. http://www.gentest.ch/index.php?content=bloodtype&langchange=en. Retrieved 2006.
- "Blood typing systems other than ABO". BloodBook.com. 2005-09-10. http://www.bloodbook.com/type-sys.html. Retrieved 2008-07-15.
- "Blood Facts - Rare Traits". LifeShare Blood Centers. http://www.lifeshare.org/facts/raretraits.htm. Retrieved September 15, 2006.
- "Modern Human Variation: Distribution of Blood Types". Dr. Dennis O'Neil, Behavioral Sciences Department, Palomar College, San Marcos, California. 2001-06-06. Archived from the original on 2006-02-21. http://web.archive.org/web/*/http://anthro.palomar.edu/vary/vary_3.htmhttp://web.archive.org/web/*/http://anthro.palomar.edu/vary/vary_3.htm. Retrieved November 23, 2006.
- "Racial and Ethnic Distribution of ABO Blood Types - BloodBook.com, Blood Information for Life". bloodbook.com. http://www.bloodbook.com/world-abo.html. Retrieved September 15, 2006.
- "Molecular Genetic Basis of ABO". http://abobloodgroup.googlepages.com/home. Retrieved July 31, 2008.
- Blood Type Calculator -The calculator is used to determine the blood type of child when the blood type of parents are known.
|
|||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||